2023 and the start of 2024 in research were full of illuminating studies and earthquaking...
Taking Stock of the Pandemic: Greatest Research Discoveries of COVID
It’s now been over three years since COVID-19 began to sweep across the world, altering lives, politics, and the global economy forever. Not to mention the pandemic’s far-reaching impacts on the worlds of research, science, and medicine.
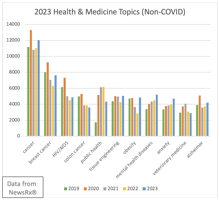
Per data from NewsRx’s BUTTER, there have been over 154,000 peer-reviewed studies on COVID-19 from 2020 to the end of 2022. That’s an absolutely astounding volume of research. In 2022, COVID-19 research kept up as strong and steady as ever, as researchers continued to unpack the far-reaching economic and health effects as well as more deeply investigate topics like long COVID and the nuances of vaccine impacts.
Nevertheless, some topics stand out above the rest. We’ve taken a deep dive into COVID-19 research to present the top five coronavirus research discoveries, debates, and topics.
#1: Airborne vs. droplet transmission
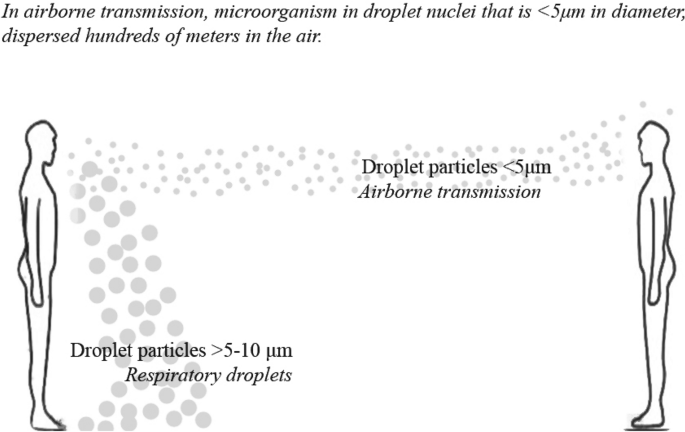
Early in the pandemic, the World Health Organization stated that SARS-CoV-2 was not transmitted through the air. It took all the way until December 2021 for the WHO to use the word “airborne” to describe the virus. At that time, the important authority recognized that transmission can occur through “long-range airborne transmission” in poorly ventilated or crowded indoor settings “because aerosols can remain suspended in the air or travel farther than conversational distance.” While large droplets settle rapidly, small aerosols can remain airborne and travel over longer distances by airflow.
Nonetheless, this matter was a real debate in the scientific community for years. A big factor was that engineering professionals involved in the study of airflow in contained environments and those who research viral infection and spread in populations had very different perspectives.
One of the first influential studies to establish that COVID-19 did in fact spread via aerosols was published in June 2020 on PNAS by Renyi Zhang, Yixin Li, Annie Zhang, and Mario Molina from Texas A&M University, the California Institute of Technology, and UC San Diego. This study found that “airborne transmission route is highly virulent and dominant for the spread of COVID-19” and that “the difference with and without mandated face covering represents the determinant in shaping the trends of the pandemic.”
This study and many others led a group of aerosol scientists, infectious-disease specialists, and building and ventilation engineers to petition the WHO and other government bodies to update their understanding of the disease’s transmission and recommend corresponding measures, including ventilation and filtration in addition to physical distancing and masking.
#2: Asymptomatic spread
An important and massively cited research letter was published in JAMA on February 21, 2020, near the very beginning of the spread of COVID-19. At the time, there were still well under 100,000 total global cases and under 3,000 total deaths. This study, from scientists in Henan, observed an asymptomatic carrier of the virus infecting others. “If the findings in this report…are replicated,” a note in the discussion states, “the prevention of COVID-19 infection would prove a challenge.” It proved true, to say the least.

Other studies went on to expand on this observation, although it was far from simple. A December 2020 study published at the BMJ discussed how it was unclear just how many infected persons were asymptomatic (early estimations of 80% were revised down to 17-20%), and it was just as unclear to what extent asymptomatic carriers transmit the disease. Early pandemic studies had shown some asymptomatic individuals infecting others; other studies did not. In January 2021, a CDC study published in JAMA estimated that transmission from asymptomatic individuals accounted for more than half of all transmission. A March 2021 Lancet study suggested that asymptomatic individuals are infectious during the early stage of the infection.
This body of research contributed significantly to our understanding of the relationships between viral load, viral shedding, infection, infectiousness, and duration of infectiousness. The findings also have important implications on public health responses to the pandemic, necessitating contact tracing and isolation for asymptomatic individuals.
#3: The rapid development of COVID-19 vaccines
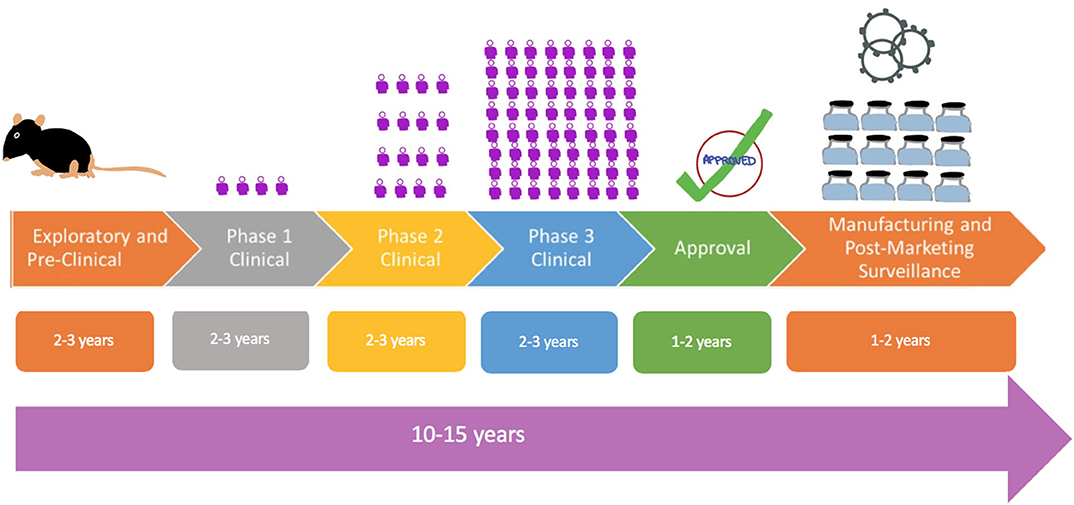
When the FDA issued emergency authorization use for the first COVID-19 vaccine in December 2020, the course of the pandemic changed forever. It’s estimated that approximately four years got chopped off the development timeline with the creation of the COVID-19 vaccine compared to traditional processes.
The timeline went roughly as follows. On January 10, 2020, scientists released the complete COVID-19 genetic blueprint. This armed researchers with the genetic instructions for making the spike proteins that the virus uses to break into the cells. The spike proteins made an easy target for the immune system to recognize, so it helped scientists hone in.
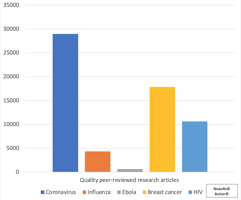
These steps happened quickly thanks to previous scientific advances. The human genome project, which took 13 years to complete, enables genome mapping today to be completed by computers in a matter of hours. Decades of studying coronaviruses after MERS and SARS outbreaks gave researchers the necessary background knowledge about spike proteins, and decades of work on HIV vaccines gave scientists potential ‘plug and play’ models of vaccines to apply to the novel coronavirus.
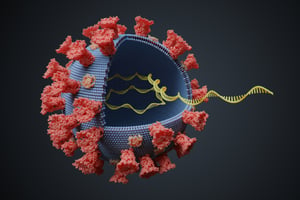
The result, at least in the case of the Pfizer and Modern vaccines, was a vaccine based on these existing templates. It carries a nonfunctional strand of viral mRNA to cells and delivers instructions of how to create copies of the foreign protein. Changes were required to make the ingredients specific to SARS-CoV-2, but nevertheless by summer 2021, a model was ready.
The most drastic time-savings came in the testing process. Many Americans were willing volunteers for testing, and it took just under 16 weeks to recruit 43,000 volunteers for testing the Pfizer vaccine. Meanwhile, COVID-19’s spread was so rapid that it allowed for a quick comparative calculation of how much the vaccine was interfering with transmission. The waiting time in the FDA’s review process was also drastically reduced: a typical 10-month wait time was cut down to just three weeks.
#4: The origin of the deadly virus
The question of COVID-19’s true origin does not yet have a definitive answer. But research has led to many clues that are essential for the world of health and science—as understanding the origins of the virus will be crucial to prevent future outbreaks.
A number of research studies in the spring and summer of 2020 provided convincing evidence for the most commonly accepted theory: that the virus originated in bats and spread to humans. In July 2020, a study out of the University of Hong Kong found evolutionarily similar viruses in bats. Although the researchers didn’t find a direct ancestral virus, they did show solid proof that COVID-19’s genome is closest to coronaviruses that infect horseshoe bats. In September 2021, researchers found three viruses in bats in Laos that were more similar to SARS-CoV-2 than any other known viruses.
Other theories have suggested a virus produced in or leaked from a laboratory, which the WHO has called “extremely unlikely” after a delegation visited Wuhan to investigate in January 2021. Nevertheless, U.S. diplomats who had previously visited the Wuhan Institute of Virology had raised concerns about vulnerabilities, and in October 2021, the U.S. Office of the Director of National Intelligence (ODNI) wrote a report stating that a lab incident was plausible. Lab leaks have happened before, after all, including a small outbreak of SARS in 2004.
Hopefully further research can pin down the origin of the virus to shed more light on the risks of human-animal interaction, selling animals, and laboratory safety.
#5: Long COVID
Research shows that nearly one in five American adults who had COVID-19 suffer from “long COVID.” Fortunately, research on developing a better understanding of the long-term effects of the virus has risen greatly in the past twelve months.
But one of the very first studies to describe long COVID as such was a research study out of the Royal Free London NHS Foundation Trust, published in November 2020 at BMJ. This study observed that nearly two months after being discharged from the hospital, high numbers of patients were experiencing breathlessness, cough, and fatigue. Others were even experiencing depression and nearly 40% retained abnormal chest radiographs.

Another early study was completed by researchers in Sweden at Karolinska Institute in the Journal of Paediatrics and Child Health. The paper followed five Swedish children with long-term symptoms, including fatigue, heart palpitations or chest pain, headaches, difficulties concentrating, muscle weakness, and more. Even after 6-8 months, none of these children had fully returned to school.
Two years later, more research still needs to be done on the long-term effects of the virus, but it is encouraging to see progress being made. Here is the latest CDC fact sheet on what we know about long COVID.
Honorable mentions
One important research area included studies that demonstrated the value of hard vs. soft lockdowns. A big data analysis published in the National Library of Medicine found that the pandemic duration under the strictest lockdown is about two months shorter than that under the lightest lockdown, leading researchers to argue that the strictest lockdowns were more epidemiologically and economically efficient. Still, scientists point out that more research needs to be done on the long-lasting knock-down economic effects and the implications of policies that cut social contact, especially for children in schools. These studies will help governments set their policy course during future pandemics.
Another worthy honorable mention is all of the research that went into finding and developing drugs to save the lives of COVID-19 patients. For example, researchers in the NIHR-funded RECOVERY study discovered that the steroid dexamethasone and the arthritis treatment tocilizumab were able to dramatically reduce the risk of death in patients suffering from severe COVID-19.
Other noteworthy studies showed how COVID-19 dealt harder blows to people with lower incomes due to factors including crowded households and an inability to work from home; others demonstrated the link between coronavirus and health conditions such as cancer complications and heart attacks.
Many of the 100,000+ pandemic-related studies deserve attention and contributed to the struggle against the virus in some way. Meanwhile, important research on long COVID, the mental health fallout of the pandemic, and the still-evolving variants of the virus continues. While the most dramatic phase of the COVID-19 pandemic is over, research that gains a better understanding of the disease and the world under its influence is just beginning.

.jpg?width=50&name=DSC_0028%20(1).jpg)